 Breathing is an integral part of the music making process, not only for singers and wind players, but for everyone. In music, the phrasing is the dictating factor of breath. Because of this, the body cannot breathe when it wants to, but when the music wants to. This requires the body to undergo forced breathing, which both requires a different part of the brain to activate, and changes the equilibrium of gas in our blood reached by automated breathing. Studies show that the changes our body undergoes during mechanical breathing impact our cognitive function; how can we as musicians use our body to make the most of, or counteract these physiological changes?
Breathing is an integral part of the music making process, not only for singers and wind players, but for everyone. In music, the phrasing is the dictating factor of breath. Because of this, the body cannot breathe when it wants to, but when the music wants to. This requires the body to undergo forced breathing, which both requires a different part of the brain to activate, and changes the equilibrium of gas in our blood reached by automated breathing. Studies show that the changes our body undergoes during mechanical breathing impact our cognitive function; how can we as musicians use our body to make the most of, or counteract these physiological changes?
In order to understand this further, and how breathing can affect the music making process, it is useful to understand how respiration works.
Studies Show, that during exercise, if a person is forced to slow their breathing, it causes a significant drop in the efficiency of the respiratory muscles. This means, that because the body isn’t getting the proper amount of oxygen, the muscles are put to a disadvantage. This of course causes a problem, because if the respiratory muscles are impaired, it inhibits them from taking adequate breaths thereafter. Have you ever noticed when you begin to run out of air in a passage, go to take a breath, and during the breath you don’t actually end up getting as much air as when you just take a regular breath? This is because the muscles are already fatigued, and the subsequent breath is only a fraction of what it could have been, had the muscles been at their full capacity.
How does air move in and out of the lungs?
[accordion multiopen=”true”]
[toggle title=”Structure of the Respiratory System” state=”opened”]
First, let’s take a look at the parts of the respiratory system:
Image by LadyofHats (Public Domain), Wikimedia Commons.
According to Gray’s basic anatomy:
Diaphragm: A large dome shaped muscle that contracts during inhalation (for more information, click here!)
Nasal Cavity: Located in the middle of the face, the nasal cavity is a large air filled space. Air travels from the nostrils into this space
Pharynx: Located behind the nasal cavity, the pharynx’s main job when it comes to respiration, is to warm and help filter the air as it enters the body
Larynx: Also known as the “voice” box, this organ contributes to respiration much like the pharynx- it helps to warm and filter the air as it enters the body
Trachea: Also known as the “windpipe” this is a tube that carries air through the body towards the lungs
Bronchi: The trachea branches into two separate tubes called the bronchi- these carry the air to each of the lungs
Bronchioles: The bronchi branch further into smaller air passages called bronchioles. This network of bronchioles hold resemblance to a tree. Their purpose is the create more surface area for gas exchange in the lungs
Alveolar sacs: Alveolar sacs hold the alveoli- which is where gas exchange occurs
[/toggle]
[toggle title=”Gas Uptake in the Blood”]
How it works:
Now, a quick physics refresher! According to Boyle’s Law: at constant temperature for a fixed mass, the absolute pressure and the volume of a gas are inversely proportional.
Image property of Arman Cagle (Own work), Wikimedia Commons
V is proportional to the inverse of P, meaning, that gases at a constant temperature will be at a higher pressure if the volume is lower, and gases will be at a lower pressure when volume is higher.
During inhalation, the diaphragm contracts downwards, creating a larger space in the lungs. This increase in volume results in a lower pressure, and since higher pressure gases always move to lower pressure in search of equilibrium, the gas from the outside atmosphere enters the lungs.
Air travels through the nasal cavity, the trachea, and then branches into smaller tubes called bronchioles. At the end of these bronchioles, you find the alveolar sacs, where gas exchange occurs. Gases pass through a thin membrane and enters the blood through diffusion.
[/toggle]
[toggle title=”Diffusion Across a Membrane”]
What is diffusion through a membrane?
One of the simplest ways to think about it, is that the substance basically dissolves into the membrane, and then undergoes the same process out of it. So the membrane is not a barrier that keeps things out, it is also a fluid substance that is constantly changing composition, depending on what is entering and leaving it. Gas exchange occurs through a process called passive diffusion, which means it does not require an external energy source. It works by means of partial pressure, where gases move from a higher pressure state to a lower pressure state on their own (much like when we inhale).
Below is a comprehensive video summarizing gas exchange:
In order for gas exchange to be done efficiently, we need two main things:
- large surface area
- very thin membrane
[/toggle]
[/accordion]
The Science:
Fick’s Law of Diffusion:
Rate of Gas Transfer = (D) (A/T) (P1-P2)
D= describes the ease at which a particular gas can pass through a particular membrane (diffusion coefficient)
A= Area of diffusion
T= thickness of the membrane
P1 and P2 are the upstream and downstream potential pressures of the gases
[accordion multiopen=”true”]
[toggle title=”What does this mean?” state=”closed”]
Essentially this means that there are 3 main factors that affect the rate of gas exchange:
1) a larger pressure difference
2) a thinner membrane
3) a larger surface area
[/toggle]
[toggle title=”Cool! I want to to know more!”]
Further information:
Diffusion Coefficient (D) = sol / √mW
Where sol is the solubility of of the gas, and mW is the molecular weight of the gas molecule.
The D value will be different for each gas because this value is dependant on the molecular weight of the particular gas. This obviously poses an issue seeing as the air that we breathe in does not only contain one type of gas. This means that CO2 and O2 have different diffusion coefficients, which is why we can have a build up of certain types of gas in the blood.
Fun Facts!
-The sheet of blood which receives oxygen through the alveolar membranes is so thin, it is only one blood cell thick!
-The term “up” and “down” stream potential pressures refers to the gases entering and leaving the membrane
[/toggle]
[/accordion]
Why do I need to know about gas diffusion and respiration?
The short answer is, you don’t. Many phenomenal musicians live their daily lives without being familiar with the intimate knowledge of how their body works, and there’s nothing wrong with that. Others, spin their wheels in the practice room, drilling passages over and over again without really getting results, and not knowing why.
While there are many studies on how exercise affects breathing, and there are a few studies (example found here) that demonstrate that the rate at which you breathe affects your cognitive function, there is little research on this phenomenon applied to musicians. Musicians have recently been becoming more interested in the “non musical” ways of practicing that have become standard practice in the athletic world. As musicians, we often equate ourselves to professional athletes, and we are beginning to treat performance anxiety the way that athletes do. The next reasonable step is to apply the research that has been done regarding regulating breathing (in sports such as swimming) and applying it to musicians that need to self regulate their breathing as well.
What happens during forced breathing?
During a musical phrase, a wind player must provide a constant (though pressure varied) stream of air to the instrument in order to produce sound. This manipulation of ventilation causes a few things to occur in the body:
[accordion multiopen=”true”]
[toggle title=”Gas Concentrations in the Blood” state=”closed”]
- The gas levels in the blood change
Ventilation is controlled by the partial pressures of gases in the blood, particularly the partial pressure of carbon dioxide. Our body receives gas through respiration, and the gas is supplied to the blood through the alveoli in the lungs. During normal breathing, our blood reaches a homeostasis that is maintained through regular breathing patterns (normal, quiet breathing, that our body does on its own), but when the body undergoes mechanical ventilation (ie, breathing that is consciously controlled) the gas levels in the blood change, and homeostasis is lost. If a person is to breathe too often (hyperventilation), they can have an excess of oxygen in their blood, and if a person’s breathing is slowed (hypoventilation) it can cause an excess of carbon dioxide to build up in the blood.
[/toggle]
[toggle title=”How does this affect us physically?” state=”closed”]
How does this affect us physically?
If a person is to deliberately slow their breaths (like when a wind musician must take make long phrases without breathing) it can cause something called hypercapnia which is an abnormally high carbon dioxide concentration in the blood. This also causes respiratory acidosis, which is essentially the pH of the blood lowering to become more acidic because of a build up of hydrogen ions. The slowed breathing process is something called hypoventilation.
A study was done, testing the affect on hypoventilation (and resulting hypercapnia) on respiratory muscle function. The study consisted of having the subjects pedal on mechanical bikes in two separate tests monitoring their ventilation. The first test allowed the subjects to breathe freely, while the second test involved a training portion where the subjects were trained to be able to lower their air intake over 3 weeks using mechanical breathing, and all but 2 were able to do this (leaving 12 subjects for the study). Researchers were then able to monitor the effectiveness of the diaphragm muscles in breathing when they were forced to slow their breaths (producing hypercapnia and respiratory acidosis in the blood) vs when they were allowed to breathe freely. The study found that 10 minutes after exercise, there was significant impairment of the diaphragm, indicating impairment of the respiratory muscles.
[/toggle]
[toggle title=”How does this affect us musically?”]
How does this affect us musically?
Believe it or not, there is evidence that shows that the concentration of CO2 in your breath can affect the pitch of a given note.
The study linked used one subject (a professional musician) playing both the oboe, and the clarinet. It was found that the concentration of CO2 in the air varies from 2.5%-8.5% depending on the length of the musical phrase, and can affect the pitch up to 30 cents. The testing was done using a small tube inserted into the corner of the player’s mouth that was connected to a machine that measured the spontaneous CO2 concentration. The change in pitch is largely attributed in the study, to the differing densities of air depending on the amount of CO2. It is alluded to, that the density of the air, in combination with other factors such as humidity, and embouchure, are the main cause of pitch variation.
[/toggle]
[toggle title=”What does this tell us about breathing?”]
What does this tell us about breathing?
If we think about the gas exchange process itself, we can draw further conclusions. CO2 buildup in the blood is something that oboists have become very familiar with. Of all the instruments, they usually know that the best breath is taken when you have had the chance to exhale before hand. Because oboists have such a small aperture to blow into, the volume of air needed is very low, and consequently they can go very long periods of time without taking a breath. Oboists therefore often plan “exhale breaths” where they breathe out instead of breathing in, in order to avoid CO2 buildup. Other instruments however, need to be aware of the danger of CO2 buildup as well.
Instruments such as tuba and flute need incredible amounts of air, and therefore need to breathe often. Many times (especially in the case of the flute) players are needed to take catch breaths (or very quick, short breaths) that are undetectable as possible. When one takes a short shallow “catch breath” they are not breathing into the lungs, but into the dead space which is the area located from the nasal cavity up to the bronchioles.
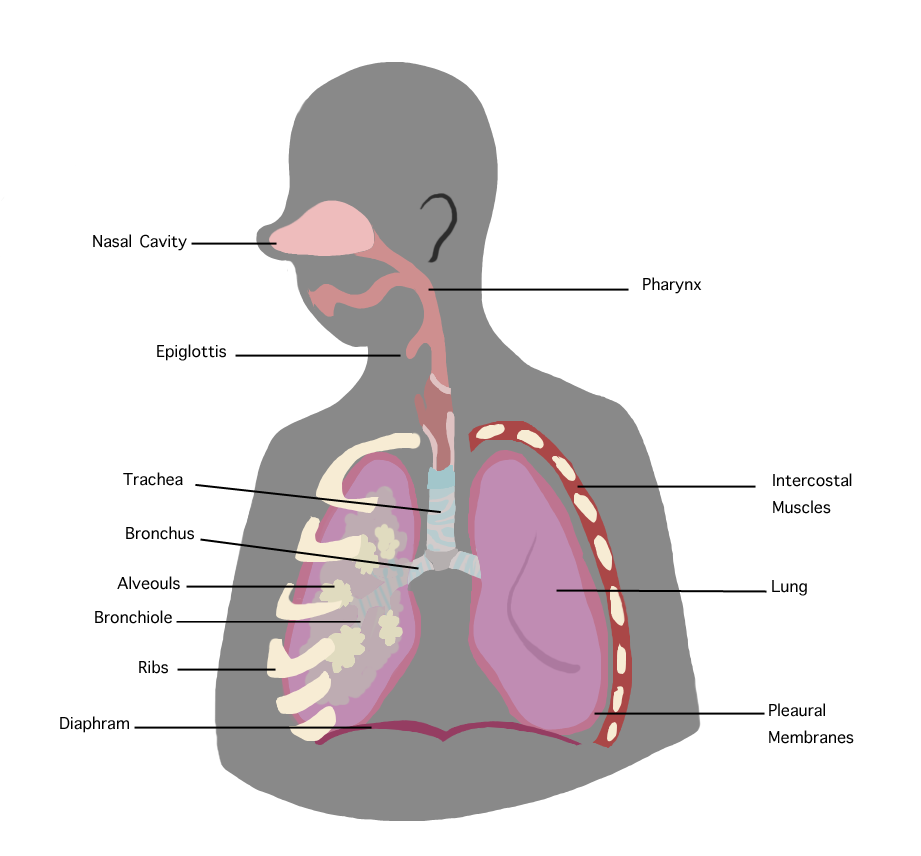
Image property of Yoshina (Own work), Wikimedia commons.
This area is called dead space because gas exchange does not occur here (gas exchange only occurs in the alveoli!). Therefore, taking short shallow breaths only temporarily aids the player in putting more air through the instrument and does not actually provide the body with the oxygen it needs. This is the reason that passages that require many short breaths are often very tiring.
[/toggle]
[toggle title=”Cognitive Function is Affected”]
2) Changes in blood gas concentration causes a change in cognitive function
In a study done on hypoventilation syndrome, scientists use a woman with a rare condition, central congenital hypoventilation syndrome (CCHS) to research the differing cognitive functions between spontaneous and mechanical breathing. In CCHS, patients have the ability to use voluntary breath during the day for ventilation, but require assistance at night for breathing as they are unable to perform automatic breathing. This study found that mechanical breathing allowed for greater cognitive function, as the frontal lobe is free from it’s duties of spontaneous ventilation. The study draws a direct correlation between control over a motor activity, and cognition.
While this suggests that wind musicians have the possibility of benefitting from freed up cognitive function, we must be careful in drawing the conclusion that forced breathing allows for more complex thought. There are other factors to consider when looking at CCHS patients (ie, oxygenation level of the blood, the fact that their autonomic system is not working at the same level as those without CCHS).
So, can forced breathing free up cognitive function that would otherwise be occupied and give musicians a greater mental capacity? POSSIBLY! Though there is not research to say definitively.
[/toggle]
[/accordion]
Now that we know that regulated, controlled breathing can benefit us as musicians, what can we do to maximize this?
While there is scientific evidence (explained above)that freeing your brain of the task of involuntary breathing can help with cognitive function, it sure doesn’t feel that way when you’re in the middle of a phrase and running out of air! In order to maximize and destress performance, it is helpful for musicians to plan ahead and foresee possible issues.
Along with hypoventilation, hyperventilation is also an issue among musicians, especially when it comes to performance anxiety. As musicians, we know that many aspects of the music making process are interconnected and that we must think of a broader picture when thinking of our health as musicians.
Practice tips:
- plan your exhales along with your inhales of breath
- practice running out of air
- practice when you are out of breath (run around, do jumping jacks ect) in order to simulate a performance situation
- Yoga: The breathing control exercises practiced in yoga can not only help with strengthening your respiratory muscles, but can also help manage the breath. If you don’t take a quality breath, it can be just as bad as not taking a breath at all. Figure out what your body needs in order to get the most out of each breath.
[accordion]
[toggle title=”References and Further Reading” state=”closed”]
Drake, R. L., Mitchell, A. W., & Vogl, W. (2012). Gray’s basic anatomy. Philadelphia: Elsevier/Churchill Livingstone.
Enson, Y. (2006). Effects of acidosis on respiratory function. Annals of the New York Academy of Sciences, 121(3), 674-690. doi: https://doi.org/10.1111/j.1749-6632.1965.tb14237.x
Gardner, W. (1992). Hyperventilation syndromes. Respiratory Medicine, 86(4), 273-275. doi:https://doi.org/10.1016/s0954-6111(06)80023-5
Gonsalez, N. (1988). Oxygen transfer from atmosphere to tissues. Advances in Experimental Medicine and Biology. doi:https://doi.org/10.1007/978-1-4684-5481-9
Fuks, L. (1996). Prediction of pitch effects from measured CO2 content variations in wind instrument playing. TMH-QPSR, 37(4), 37-43.
Jonville, S., Delpech, N., & Denjean, A. (2002). Contribution of respiratory acidosis to diaphragmatic fatigue at exercise. European Respiratory Journal, 19(6), 1079-1086. doi:https://doi.org/10.1183/09031936.02.00268202
Khalsa, S. B., Shorter, S. M., Cope, S., Wyshak, G., & Sklar, E. (2009). Yoga ameliorates performance anxiety and mood disturbance in young professional musicians. Applied Psychophysiology and Biofeedback, 34(4), 279-289. doi:https://doi.org/10.1007/s10484-009-9103-4
McConnell, A., Gosselink, H., & Hogarth, B. (2013). Respiratory muscle training: Theory and practice. Edinburgh: Churchill Livingstone Elsevier. doi:https://doi.org/10.1016/b978-0-7020-5020-6.00004-2
Propert, D. (2014). Recognizing and treating breathing disorders – A Multidisciplinary Approach. International Journal of Osteopathic Medicine, 17(3), 216-217. doi:https://doi.org/10.1016/j.ijosm.2014.04.006
Sharman, M., Gallea, C., Lehongre, K., Galanaud, D., Nicolas, N., Similowski, T., Naccache, L. (2014). The cerebral cost of breathing: An fMRI case-study in congenital central hypoventilation syndrome. PLoS ONE, 9(9). doi:https://doi.org/10.1371/journal.pone.0107850
Studer, R., Danuser, B., Hildebrandt, H., Arial, M., & Gomez, P. (2011). Hyperventilation complaints in music performance anxiety among classical music students. Journal of Psychosomatic Research,70(6), 557-564. doi:https://doi.org/10.1016/j.jpsychores.2010.11.004
[/toggle]
[/accordion]
[accordion]
[toggle title=”Image List” state=”closed”]
“Question guy” figure: clipart, “https://openclipart.org/detail/191766/question-guy”
Respiratory System figure: By LadyofHats [Public domain], via Wikimedia Commons: https://upload.wikimedia.org/wikipedia/commons/5/5e/Respiratory_system_complete_en.svg
Boyle’s Law figure: Image property of Arman Cagle (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons
Dead Space figure: Image property of Yoshina (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons
[/toggle]
[/accordion]
